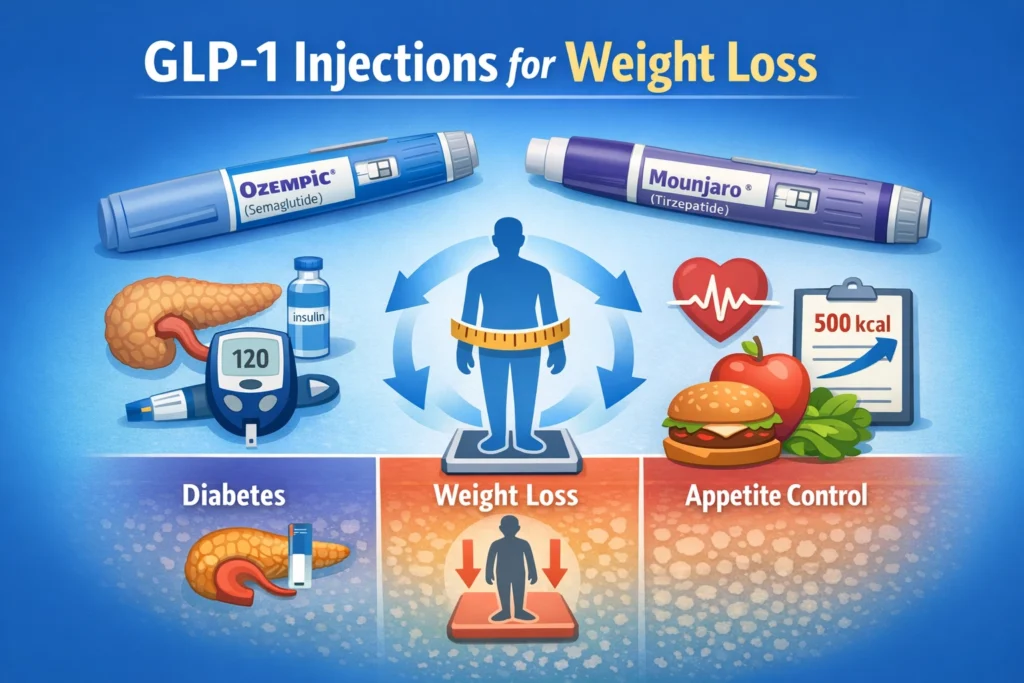
GLP-1 injections such as Ozempic and Mounjaro have become some of the most talked-about medications in the world of weight loss and metabolic health. Originally developed to treat type 2 diabetes, these medications are now widely used for weight loss—but are they a long-term solution?
This article explores how GLP-1 medications work, who they may benefit, their risks and side effects, and why experts emphasize that they are not a permanent fix for obesity.
Public discussions around GLP-1 medications have increased significantly in recent years. In a recent media interview conducted by Turkish journalist Nevşin Mengü, Dr. Nowzaradan, a well-known bariatric surgeon featured on a popular television program, shared his general perspective on GLP-1 injections. His comments highlighted both their usefulness in specific cases and their limitations as a long-term weight-loss solution.
What Are GLP-1 Injections?
GLP-1 (glucagon-like peptide-1) receptor agonists are medications designed to help regulate blood sugar in people with type 2 diabetes. Popular examples include Ozempic (semaglutide) and Mounjaro (tirzepatide).
These medications:
- Reduce the need for insulin in diabetic patients
- Improve blood sugar control
- Increase satiety (feeling full)
- Reduce appetite and caloric intake
Because patients eat less, weight loss often occurs as a secondary effect.
How Do Ozempic and Mounjaro Help With Weight Loss?
GLP-1 medications slow gastric emptying and act on appetite centers in the brain. As a result:
- Patients feel full sooner
- Cravings are reduced
- Portion sizes decrease naturally
For individuals who are not candidates for bariatric surgery, GLP-1 injections can offer a medically supervised way to initiate weight loss.
Who Can Benefit From GLP-1 Medications?
GLP-1 injections may be beneficial for:
- Patients with type 2 diabetes
- Individuals with obesity who are not eligible for surgery
- Patients needing short-term metabolic improvement
In these cases, GLP-1 therapy can be a useful jumpstart to weight loss under medical supervision.
Side Effects and Risks of GLP-1 Injections
Despite their benefits, GLP-1 medications are associated with significant side effects, which must be carefully considered.
Reported side effects include:
- Gallbladder stones
- Pancreatitis
- Acid reflux and severe nausea
- Aspiration during sleep
- Common gastrointestinal symptoms such as nausea, vomiting, acid reflux, constipation, and discomfort have been widely reported with GLP-1 medications.
Cost of Ozempic and Mounjaro: A Long-Term Issue
Another major limitation of GLP-1 injections is cost. When taken continuously over one to two years, the total expense of these medications may exceed the cost of bariatric or metabolic surgery.
For many patients, long-term affordability becomes a barrier to continued treatment.
Do You Gain Weight After Stopping GLP-1 Medications?
Clinical studies consistently show that most patients regain weight within a year after stopping GLP-1 injections.
These medications are effective only while they are being used. Once discontinued:
- Appetite returns
- Eating patterns revert
- Weight regain is common
This makes GLP-1 therapy a temporary solution, not a durable cure for obesity.
Are GLP-1 Injections a Sustainable Weight Loss Solution?

Experts emphasize that obesity is a chronic, complex disease. Like many diets or short-term interventions, GLP-1 medications often fail to deliver sustainable results when used alone.
Just as millions of people start diets after the holidays and abandon them months later, weight loss strategies that rely solely on temporary measures rarely succeed long-term.
GLP-1 Injections vs Bariatric Surgery
While GLP-1 medications have an important role, bariatric surgery remains the most durable and effective treatment for obesity in appropriate candidates. More information about bariatric surgery is available here.
Surgery:
- Produces long-term weight loss
- Improves or resolves diabetes
- Reduces obesity-related health risks
GLP-1 injections may complement treatment but should not always replace definitive options.
Public Health and Regulatory Information
This article is based on publicly available information from regulatory and public health organizations. The sources below provide general background on GLP-1 medications, their approved uses, and observed outcomes, without offering individual medical guidance.
- U.S. Food & Drug Administration (FDA) – General information on GLP-1 medications, approvals, and safety monitoring
https://www.fda.gov/drugs - National Institutes of Health (NIH) – Research summaries and publications related to GLP-1 medications and weight outcomes
https://www.ncbi.nlm.nih.gov - American Diabetes Association (ADA) – Educational resources on diabetes medications and metabolic health
https://diabetes.org
Final Thoughts: Understanding the Role of GLP-1 Medications
GLP-1 injections such as Ozempic and Mounjaro play an important role in modern diabetes care and can support short-term weight loss for selected individuals. However, current evidence shows that their effects are temporary and dependent on continuous use.
These medications may help some people initiate weight loss, especially when surgery is not an option, but they are not designed as a permanent solution for obesity. Cost, side effects, and weight regain after discontinuation remain key limitations.
For long-term health outcomes, sustainable strategies should always be discussed with qualified healthcare professionals and tailored to individual needs.
For individuals exploring non-surgical approaches, GLP-1 therapy may be considered as part of broader weight-loss treatment options under professional guidance.
Disclaimer:
This content is provided for informational and educational purposes only and is not intended as medical advice. It does not replace consultation with a qualified healthcare professional. Any decisions regarding medical treatment or medication should be made in consultation with a licensed physician.


